[vc_row][vc_column width=”1/1″][vc_column_text]
1. Introduction to Blepharoplasty
1.1 What Is Blepharoplasty?
Blepharoplasty is a type of cosmetic or functional eye lift surgery designed to remove excess skin, fat, or muscle from the upper and lower eyelids. It helps improve eye contour and rejuvenates facial appearance.
1.2 Why Eyelid Surgery Is Gaining Popularity
With minimal downtime and impressive aesthetic results, eyelid surgery is becoming one of the most sought-after facial enhancements. It addresses tired-looking eyes, puffiness, and even vision obstruction.
1.3 Cosmetic vs Functional Blepharoplasty
Cosmetic blepharoplasty is performed to enhance appearance, while functional surgery is recommended to restore impaired vision due to drooping eyelids. Both offer life-enhancing benefits.[/vc_column_text][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255147770{margin-top: -50px !important;}”][vc_column width=”1/1″][vc_custom_heading]
2. Types of Eyelid Surgery
[/vc_custom_heading][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255166050{margin-top: -50px !important;}”][vc_column width=”1/1″][vc_single_image media=”85063″ media_width_percent=”100″ border=”yes”][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255180049{margin-top: -50px !important;}”][vc_column width=”1/1″][vc_column_text]Eyelid surgery is not one-size-fits-all. It includes several targeted procedures based on the location and purpose of treatment. The main types include upper eyelid blepharoplasty, lower eyelid surgery, and combined or medically indicated surgeries. Each has distinct goals and techniques to address sagging, puffiness, or impaired vision. Whether for cosmetic enhancement or functional improvement, the right procedure is determined by individual needs and an experienced surgeon’s evaluation.
2.1 Upper Eyelid Blepharoplasty
- Definition and Purpose Upper eyelid blepharoplasty newcastle involves the removal of excess skin and fat to correct hooding and restore a youthful eye contour.
- Common Concerns Treated This procedure treats sagging lids, wrinkles, and vision obstruction caused by drooping upper eyelids.
2.2 Lower Blepharoplasty Eyelid Surgery
- What It Addresses Lower blepharoplasty eyelid surgery targets under-eye bags, puffiness, and skin laxity that contribute to a tired or aged appearance.
- Techniques Used Common techniques include transconjunctival (scarless) and subciliary (skin-based) approaches for tailored results.
2.3 Upper Eyelid Plastic Surgery vs Upper Lid Eye Surgery
- Medical vs Aesthetic Focus Upper lid surgery for medical purposes focuses on improving vision, while plastic surgery prioritizes cosmetic improvement.
- Combined Eyelid Procedures Both upper and lower blepharoplasty can be performed together for comprehensive eye rejuvenation.
[/vc_column_text][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755256145400{margin-top: -50px !important;}”][vc_column width=”1/1″][vc_custom_heading]
3. Candidacy and Eligibility
[/vc_custom_heading][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755256210570{margin-top: -50px !important;}”][vc_column width=”1/1″][vc_column_text]Determining whether you’re a good candidate for blepharoplasty involves assessing your health, eye anatomy, and aesthetic or functional concerns. Ideal candidates are generally healthy adults bothered by drooping upper lids or under-eye puffiness. A consultation with a surgeon will help evaluate your goals, discuss potential risks, and set realistic expectations based on your unique anatomy.
3.1 Who Should Consider Blepharoplasty?
Ideal candidates include individuals with drooping eyelids, excess skin, puffiness, or impaired vision from sagging lids.
3.2 Age, Skin Type, and Medical Factors
Most patients are over 35, but younger candidates with hereditary eye bags also qualify. Good overall health is key.
3.3 Contraindications and Risk Factors
Conditions like dry eyes, glaucoma, or bleeding disorders may affect eligibility. A full medical assessment is essential.[/vc_column_text][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755256162791{margin-top: -50px !important;}”][vc_column width=”1/1″][vc_custom_heading]
4. Cost of Blepharoplasty
[/vc_custom_heading][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755256283967{margin-top: -50px !important;margin-bottom: 50px !important;}”][vc_column width=”1/1″][vc_column_text]Understanding the cost of blepharoplasty helps you prepare for the financial aspect of surgery. Prices vary depending on location, surgeon’s experience, and whether you need upper, lower, or both lids treated. While some cases are medically necessary and partially covered by insurance, cosmetic procedures are typically paid out of pocket or financed through clinic-offered plans.
4.1 Average Blepharoplasty Cost by Region
In the UK, blepharoplasty ranges from £2,000 to £4,000. Costs vary based on the surgeon, facility, and procedure complexity.
But at Eldon Aesthetics it is very affordable and it only ranges from £ 1500 to £ 2000.
4.2 Factors Influencing the Price
Prices are influenced by anaesthesia, surgeon expertise, pre/post-op care, and whether one or both lids are treated.
4.3 Insurance and Financing Options
Functional blepharoplasty may be partially covered by insurance. Many clinics offer payment plans for affordability.[/vc_column_text][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255246915{margin-top: -80px !important;}”][vc_column width=”1/1″][vc_custom_heading]
5. Consultation and Preoperative Process
[/vc_custom_heading][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755256243858{margin-top: -50px !important;}”][vc_column width=”1/1″][vc_column_text]Before undergoing blepharoplasty consultation , is essential. Your surgeon will assess your medical history, current eye condition, and aesthetic preferences. You may need certain eye tests and pre-op instructions to ensure safety and effectiveness. Being prepared for surgery with a personalised plan enhances your comfort and the likelihood of a smooth recovery and optimal results.
5.1 Initial Consultation and Expectations
A detailed consultation includes medical history, visual tests, and aesthetic goals. Photos may be taken for comparison.
5.2 Pre-Surgical Evaluations and Tests
Vision checks, tear production tests, and overall health screenings are conducted to ensure surgical readiness.
5.3 Preparing for Surgery: Do’s and Don’ts
Avoid smoking, alcohol, and certain medications before surgery. Arrange for post-op support and follow instructions closely.[/vc_column_text][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755256303080{margin-top: -50px !important;}”][vc_column width=”1/1″][vc_custom_heading]
6. The Blepharoplasty Procedure
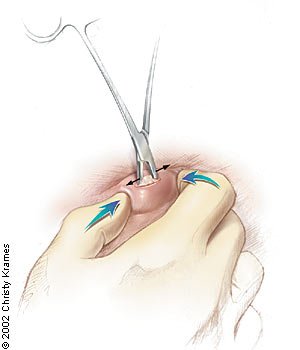
[/vc_custom_heading][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255278401{margin-top: -50px !important;}”][vc_column width=”1/1″][vc_single_image media=”85064″ media_width_percent=”100″ border=”yes”][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755253344477{margin-top: -30px !important;}”][vc_column width=”1/1″][vc_column_text]Blepharoplasty procedure (process) is performed under local or general anaesthesia, depending on the case complexity. The surgeon carefully removes or repositions skin, fat, and muscle to achieve a more youthful, refreshed appearance.
6.1 Surgical Steps for Upper Eyelid Blepharoplasty
The surgeon marks the incision line, removes excess tissue, and closes with fine sutures. Local anaesthesia is commonly used.
6.2 Procedure Breakdown for Lower Eyelid Surgery
The approach for lower eyelid surgery depends on fat distribution and skin laxity. Fat may be repositioned, and skin tightened for a smoother contour.
6.3 Duration, Anesthesia, and Pain Management
Blepharoplasty takes 1–2 hours. Local anaesthesia with sedation ensures comfort. Pain is minimal and well managed post-op.[/vc_column_text][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755256335921{margin-top: -50px !important;}”][vc_column width=”1/1″][vc_custom_heading]
7. Postoperative Recovery Process
[/vc_custom_heading][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755256322871{margin-top: -50px !important;}”][vc_column width=”1/1″][vc_column_text]The postoperative recovery process for blepharoplasty involves mild swelling, bruising, and discomfort, which typically subside within 1–2 weeks. Following your surgeon’s aftercare instructions ensures proper healing, reduces complications, and helps achieve optimal results from your eyelid surgery.
7.1 Recovery Timeline: Day 1 to Week 6
Swelling and bruising peak within the first week. Stitches are removed in 5–7 days. Most results become visible after 2 weeks.
7.2 Tips to Reduce Swelling and Bruising
Apply cold compresses, keep the head elevated, and avoid strenuous activity for optimal healing and minimal bruising.
7.3 When to Resume Daily Activities and Work
Light activities can resume within a few days. Most return to work in 7–10 days. Full recovery takes 4–6 weeks.[/vc_column_text][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255334937{margin-top: -80px !important;}”][vc_column width=”1/1″][vc_custom_heading]
8. Expected Results and Longevity
[/vc_custom_heading][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255593713{margin-top: -70px !important;}”][vc_column width=”1/1″][vc_column_text]Blepharoplasty offers lasting results, with most patients enjoying a brighter, rejuvenated eye appearance for years. Results start becoming visible within weeks and continue to improve over time. Although the ageing process continues, the effects of eyelid surgery are long-lasting.
8.1 How Soon Will You See Results?
Initial results appear after swelling subsides in 1–2 weeks. Final results are visible by the 6-week mark.
8.2 Before-and-After Expectations
You’ll notice a more open, rested appearance with natural-looking results that preserve your facial character.
8.3 How Long Do Results Last?
Results typically last 5–10 years. Ageing continues naturally, but lifestyle and skincare can help maintain effects.[/vc_column_text][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255356346{margin-top: -80px !important;}”][vc_column width=”1/1″][vc_custom_heading]
9. Risks and Complications
[/vc_custom_heading][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255606673{margin-top: -70px !important;}”][vc_column width=”1/1″][vc_column_text css=”.vc_custom_1755536028793{margin-bottom: 20px !important;}”]Like any surgical procedure, blepharoplasty carries some risks. While most side effects are mild and temporary—such as swelling or bruising—complications like infection or asymmetry can occur. Choosing a qualified and experienced surgeon greatly reduces these risks. Patients should follow all medical advice before and after surgery to ensure the safest and most successful outcome.
9.1 Common Side Effects (Swelling, Dry Eyes)
Temporary swelling, bruising, dry eyes, or tightness are common and resolve within weeks.
9.2 Rare But Serious Complications
Rare risks include infection, asymmetry, vision changes, or scarring. Choosing a skilled surgeon reduces these risks.
9.3 How to Minimize Risks
Follow pre- and post-op instructions, avoid smoking, and select a qualified blepharoplasty clinic in Newcastle upon Tyne.[/vc_column_text][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755535977120{margin-top: -60px !important;}”][vc_column width=”1/1″][vc_custom_heading]
10. Non-Surgical Alternatives
[/vc_custom_heading][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255620426{margin-top: -70px !important;}”][vc_column width=”1/1″][vc_column_text]
Dermal fillers can temporarily improve hollow under-eyes but do not remove excess skin.
-
Laser Resurfacing for Eyelid Tightening
Laser treatments tighten surface skin but are not effective for fat bulges or significant drooping.
-
When Surgery Is the Better Option
Surgery remains the gold standard for lasting, dramatic improvements that non-invasive methods can’t match.[/vc_column_text][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255387419{margin-top: -80px !important;}”][vc_column width=”1/1″][vc_custom_heading]
11. Psychological Impact and Self-Confidence
[/vc_custom_heading][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255652673{margin-top: -70px !important;}”][vc_column width=”1/1″][vc_column_text]
-
Boosting Confidence Post-Surgery
Many patients report improved self-esteem and confidence due to a more rested and rejuvenated appearance.
-
Managing Expectations Emotionally
Counselling or clear communication with your surgeon helps ensure your goals align with achievable outcomes.[/vc_column_text][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255402256{margin-top: -80px !important;}”][vc_column width=”1/1″][vc_custom_heading]
12. Lifestyle Adjustments Post-Surgery
[/vc_custom_heading][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255684251{margin-top: -70px !important;}”][vc_column width=”1/1″][vc_column_text]
-
Skincare and Eye Care Tips
Use gentle, non-irritating products and sun protection. Hydration and regular skincare maintain surgical results.
-
Protecting Your Eyes from Sun and Irritants
Wear sunglasses, avoid dusty environments, and limit screen time during early healing.[/vc_column_text][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255419954{margin-top: -80px !important;}”][vc_column width=”1/1″][vc_custom_heading]
13. Revision and Secondary Blepharoplasty
[/vc_custom_heading][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255719937{margin-top: -70px !important;}”][vc_column width=”1/1″][vc_column_text]In some cases, a revision procedure may be necessary to refine results or correct issues from a previous surgery. Whether due to healing complications or changes in anatomy over time, secondary blepharoplasty is typically safe when performed by a skilled surgeon. Patients should wait for full healing before considering further surgery to achieve optimal outcomes.
13.1 When Revisions Are Necessary
Revisions may be needed for asymmetry, excess skin, or unsatisfactory results. It’s generally safe after full healing.
13.2 What to Expect from a Second Surgery
Secondary surgeries require precise planning and may involve scar tissue adjustment. Outcomes can still be excellent.[/vc_column_text][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255736842{margin-top: -80px !important;}”][vc_column width=”1/1″][vc_custom_heading]
14. Myths vs Facts About Eyelid Surgery
[/vc_custom_heading][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255748272{margin-top: -70px !important;}”][vc_column width=”1/1″][vc_column_text]
14.1 “It’s Only Cosmetic” – and Other Myths
Blepharoplasty also has functional benefits, especially for those with vision interference due to drooping lids.
14.2 Evidence-Based Truths
Research shows the procedure is safe, effective, and highly satisfying for suitable candidates.[/vc_column_text][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255765770{margin-top: -80px !important;}”][vc_column width=”1/1″][vc_custom_heading]
Conclusion
[/vc_custom_heading][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255779073{margin-top: -70px !important;}”][vc_column width=”1/1″][vc_column_text]Blepharoplasty, commonly known as eyelid surgery, is a safe and effective procedure designed to rejuvenate the eyes by removing excess skin, fat, or muscle from the upper or lower eyelids. It can be performed for cosmetic enhancement or functional improvement, such as correcting vision obstruction. With various surgical and non-surgical options, a personalised approach, and minimal recovery time, blepharoplasty offers long-lasting aesthetic and medical benefits for suitable candidates.
Ready to Rejuvenate Your Eyes?
If you’re considering blepharoplasty in Newcastle Upon Tyne, trust the expert team at Eldon Aesthetics & Skin Surgery Clinic—a CQC-registered clinic known for safe, affordable, and natural-looking results. Whether you’re looking to restore your confidence or improve vision, our specialists will guide you through every step with personalised care.[/vc_column_text][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255791624{margin-top: -80px !important;}”][vc_column width=”1/1″][vc_custom_heading]
FAQs
[/vc_custom_heading][/vc_column][/vc_row][vc_row row_height_percent=”0″ overlay_alpha=”50″ gutter_size=”3″ column_width_percent=”100″ shift_y=”0″ z_index=”0″ css=”.vc_custom_1755255805002{margin-top: -70px !important;}”][vc_column width=”1/1″][vc_column_text]
Is blepharoplasty painful?
Most patients report minimal discomfort thanks to modern anaesthesia and pain management.
Can both eyelids be treated at once?
Yes, upper and lower blepharoplasty can be performed in one session for comprehensive results.
How long do the results last?
Results typically last 5–10 years, with many enjoying benefits beyond that.
Will there be visible scars?
Scars are well-hidden in natural creases and fade significantly over time.
What’s the ideal age for blepharoplasty?
There’s no strict age limit, but most patients are in their 40s to 70s and have noticeable eyelid concerns.[/vc_column_text][/vc_column][/vc_row]